The Know AML website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and Know AML cannot guarantee the accuracy of translated content. Know AML and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help. The interviews webpage also uses YouTube, where subtitles and translations are generated automatically by AI; please be advised to exercise caution when precise interpretation is required. For further support with YouTube, visit YouTube Help.
Know AML webinar | Empowering patients to ask their physician the right questions during their AML journey
Gail Roboz
May 23, 2025
Know AML hosted a webinar for patients and healthcare professionals (HCPs) on April 23, 2025, titled ‘Mutation testing in AML: What you need to know’. Here, we share a discussion between Gail J. Roboz, physician at Weill Cornell Medicine and Know AML Ambassador, and Ralph Hills, Know AML Chair, where they considered the range of genetic mutations in AML and what they mean for treatments, and also how mutation testing methods used in the diagnosis of AML have changed in over the years.
They went on to debate challenges faced by patients during an AML diagnosis, including access to mutation testing and discussions between physicians and patients. They concluded by describing the importance of shared decision-making, and the role of physicians and patients in enabling clearer conversations about mutation testing in AML going forward.
Key points
- The estimated number of new cases of AML in the US in 2024 was 20,800 – 1% of all new cancer cases in the US. Survival rates have improved steadily over the past 50 years.
- Since 2017, many drugs designed to target specific mutations have been approved by the U.S. Food and Drug Administration (FDA) and the European Union (EU).
- Patients face several challenges during the process of being diagnosed with AML, including lack of awareness of testing methods, the wait time for test results, and accessing appropriate testing methods; therefore, clear communication between physicians and patients is essential.
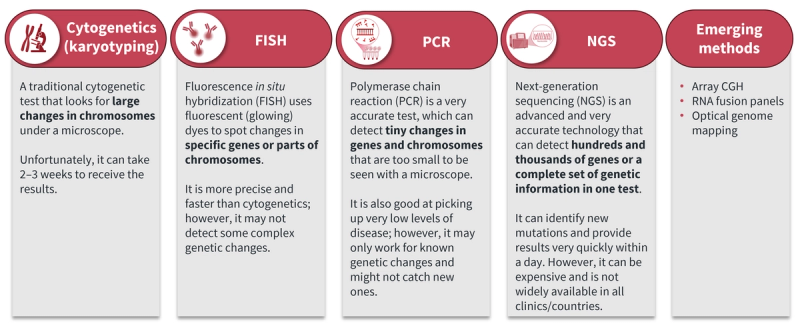
- Several mutation testing methods are available, including conventional cytogenetics (karyotyping), fluorescence in situ hybridization (FISH), polymerase chain reaction (PCR), and next-generation sequencing (NGS), and these techniques continue to evolve (Figure 1).
- Physicians play a vital role in guiding patients towards appropriate diagnostic tests needed to inform treatment decisions. Providing access to testing methods, whether as part of diagnosis and monitoring in clinics or through clinical trials, is important. For example, the US myeloMATCH trial uses NGS mutation testing to assign patients to treatments that target their specific mutations and then tests how well and safely these treatments work.
- Shared decision-making between physicians and patients is crucial to set realistic expectations for treatment and recovery, improve results following treatments, and help patients to feel more confident, independent, and in control of their health (Figure 2).

This independent educational activity is supported by Thermo Fisher Scientific.
All content was developed independently by the faculty. The funder was allowed no influence on the content.